Researchers evaluated the effectiveness of an immunotherapy method for treating cancer called CPI, using a trove of patient data. They set out to identify the variables that distinguish patients with favorable outcomes using data from a public database, finding 5 key factors to CPI response.
By María Rocha-Acevedo
Cancer is, without a doubt, one of the biggest health concerns worldwide. Countless scientists work tirelessly every day to find life-saving answers for those affected by this elusive disease. But what if we could use the body’s own defense mechanisms to fight cancer? Hundreds of years of investigation around this question evolved into one of today’s fastest-growing areas of research and a novel form of treatment: immunotherapy.
One novel form of immunotherapy works by tricking the immune system, deactivating its “turn-off” signals and allowing it to attack cancer cells. The immune system has checkpoints to prevent it from becoming too strong, protecting healthy cells. However, immune checkpoint inhibitors (CPI) can be used to stop the body from sending these “off” signals, allowing the immune system to kill cancer cells.
While CPI has provided hope and functional treatments to many patients, this form of treatment doesn’t always work as expected. In some cases, it can even have adverse effects, causing autoimmune diseases, which cause the body’s immune system to attack itself. For this reason, a group of scientists at Barcelona’s Institute for Research in Biomedicine set out to understand what distinguishes patients who respond positively to CPI from those who don’t. Dr. Abel Gonzalez-Perez and Dr. Nuria Lopez-Bigas led this research team, publishing their work in the journal Nature Genetics.
Public databases: the “big picture” for cancer research and immunotherapy
There is tons of active research on CPI, but most of the existing studies focus on a small group of tumor characteristics, like a small group of genes. This is a helpful first step, but it’s like looking at one or two trees in a forest; cancer treatment is extremely complex and many different variables need to be considered, especially when safe outcomes are a life-or-death matter. This motivated the research group of Dr. Lopez-Bigas to look at a public database generated by the Dutch Hartwig Medical Foundation.
When it comes to studying cancer, it is essential to know as many variables as possible, because every tumor is unique. It is also important to make this data available to as many researchers as possible, as there are many ways to look at a dataset. As they say, two (or many) heads think better than one. Or, when it comes to analyzing biomedical data, many research groups think better than one.
RELATED: The Cancerous Relationship Between Tumors and Grief
Therefore, the Hartwig Medical Foundation created a resource with data from hundreds of patients from the Netherlands. After obtaining the informed consent of the patients, they took and froze biopsies, which they later analyzed with DNA sequencing technology to extract as much data as possible. Furthermore, these patients’ physicians can enrich the data with information about their treatment and its results. Armed with this dataset, and like connecting the pieces to a gigantic puzzle, Dr. Lopez-Bigas’s team analyzed over 20,000 different variables to better understand why only some patients benefit from CPI immunotherapy treatment, while others don’t.
Filtering the noise: the five key factors behind CPI immunotherapy success
The analysis yielded hundreds of features associated with CPI response. While each of them represented an important clue behind the success of the immunotherapy treatment, the underlying challenge was to find large-scale patterns, summarizing this amount of information as much as possible. Using computational analysis and mathematical modeling, Dr. Lopez-Bigas’s team finally identified five key factors associated to the success of CPI:
- Tumor mutational burden. This is essentially the number of genetic mutations that a tumor has—the more mutations, the more “different” the tumor will be from the body, and hence, the more likely it is to be recognized by the immune system as a problem.
- Previous treatment. Patients who have received different treatments before CPI tend to have a less positive response. According to the researchers, it could be that the lack of success in previous treatments was caused by an aggressive tumor or by a deteriorated condition of the patient.
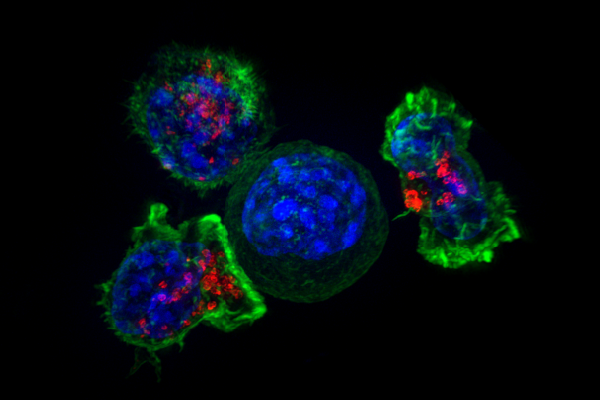
- T-cell infiltration. T-cells are one of the most important players in our body’s immune response. They are in charge of detecting and targeting threats to our health. In some cases, a certain amount of T-cells manages to sneak into a tumor; the higher this T-cell infiltration is, the more likely it is for a patient to have a positive response to CPI.
- Proliferative potential. In other words, how aggressive the tumor is, or how fast it grows. Patients with more aggressive tumors tend to have less positive responses to CPI.
- TGF-Beta activity. Transforming Growth Factor Beta (TGF-Beta) is a molecule that sends signals across cells, influencing their activity. A high activity of TGF-Beta is linked with a reduced immune response, which lowers the chances of survival after immunotherapy treatment.
Exceptions to the rule: putting criteria to the test
Tumor mutational burden (TMB) is already used in clinics to estimate the success of immunotherapy before making important clinical decisions. However, Lopez-Bigas’s team reassessed how good of a predictor TMB really is. They found out that only 42 percent of the patients with a high tumor mutational burden, according to the clinical threshold, had a positive response to CPI. The clinical threshold wasn’t as accurate as expected! On the other hand, the researchers found that using a model that combines their five key factors, 63 percent of the patients estimated to have a positive response to CPI matched the prediction.
However, no model is perfect. They found two exceptions to the assumptions of their own model. Specifically, on two cancer types: in the case of lung cancer, T-cell infiltration is not linked to CPI success. In addition, previous treatments don’t seem to affect CPI response for patients with bladder cancer. Other than these exceptions, however, these factors seem to affect the response to CPI rather predictably across different types of cancer.
Next, the group asked if these results are exclusive to CPI or if they can be generalized to any type of cancer treatment. So they went back to the dataset and found out that, while tumor mutational burden, T-cell infiltration, and TGF-Beta only seem to affect the response to CPI, proliferative potential and previous treatment seem to be predictors of response to both CPI and non-CPI cancer treatments.
RELATED: An Added Boost for Last-Ditch Cancer Treatment
It is essential to be able to identify those patients who are unlikely to respond positively to CPI, as this can help spare them from potential adverse effects of the treatment. This research has revealed life-saving information to aid in the treatment of cancer, bringing hope to improve the likelihood of patient survival.
This study was published in the peer-reviewed journal Nature Genetics.
References
National Cancer Institute. (2022, April 7). Immune checkpoint inhibitors. https://www.cancer.gov/about-cancer/treatment/types/immunotherapy/checkpoint-inhibitors
Priestley, P., Baber, J., Lolkema, M. P., … & Cuppen, E. (2019). Pan-cancer whole-genome analyses of metastatic solid tumours. Nature, 575, 210–216. https://doi.org/10.1038/s41586-019-1689-y
Sun, L., Su, Y., Jiao, A. … & Zhang, B. (2023). T cells in health and disease. Signal Transduction and Targeted Therapy, 8, 235. https://doi.org/10.1038/s41392-023-01471-y
Usset, J., Rosendahl Huber, A., Andrianova, M. A., … & Lopez-Bigas, N. (2024). Five latent factors underlie response to immunotherapy. Nature Genetics, 56, 2112–2120. https://doi.org/10.1038/s41588-024-01899-0
Waldman, A. D., Fritz, J. M., & Lenardo, M. J. (2020). A guide to cancer immunotherapy: from T cell basic science to clinical practice. Nature Reviews Immunology, 20, 651–668. https://doi.org/10.1038/s41577-020-0306-5
Featured image: Superresolution image of a group of killer T-cells (green and red) surrounding a cancer cell (blue, center). In T-cell infiltration, T-cells will attach to a cancer cell and release chemicals to kill it. Killer T cells surround a cancer cell by Alex Ritter, Jennifer Lippincott Schwartz, and Gillian Griffiths, National Institutes of Health. Image available through PDM 1.0.

About the Author
María Rocha-Acevedo is a doctoral researcher in biology, specializing in epigenetics and chromatin regulation. Her work integrates experimental and computational approaches to investigate the mechanisms of gene regulation. She is also passionate about science communication, with a focus on sharing scientific knowledge in engaging and accessible ways. Follow her on LinkedIn: https://www.linkedin.com/in/maria-rocha-acevedo/.