Antipsychotic drugs can increase the risk of diabetes, but dopamine receptors in the brain and body may be the key to a solution.
By Kyle Hewitt
Antipsychotic drugs are widely prescribed to manage mental health conditions such as schizophrenia and bipolar disorder. Unfortunately, these drugs also increase the risk of developing type 2 diabetes. A recent study might offer a potential solution.
The Problem with Antipsychotic Drugs
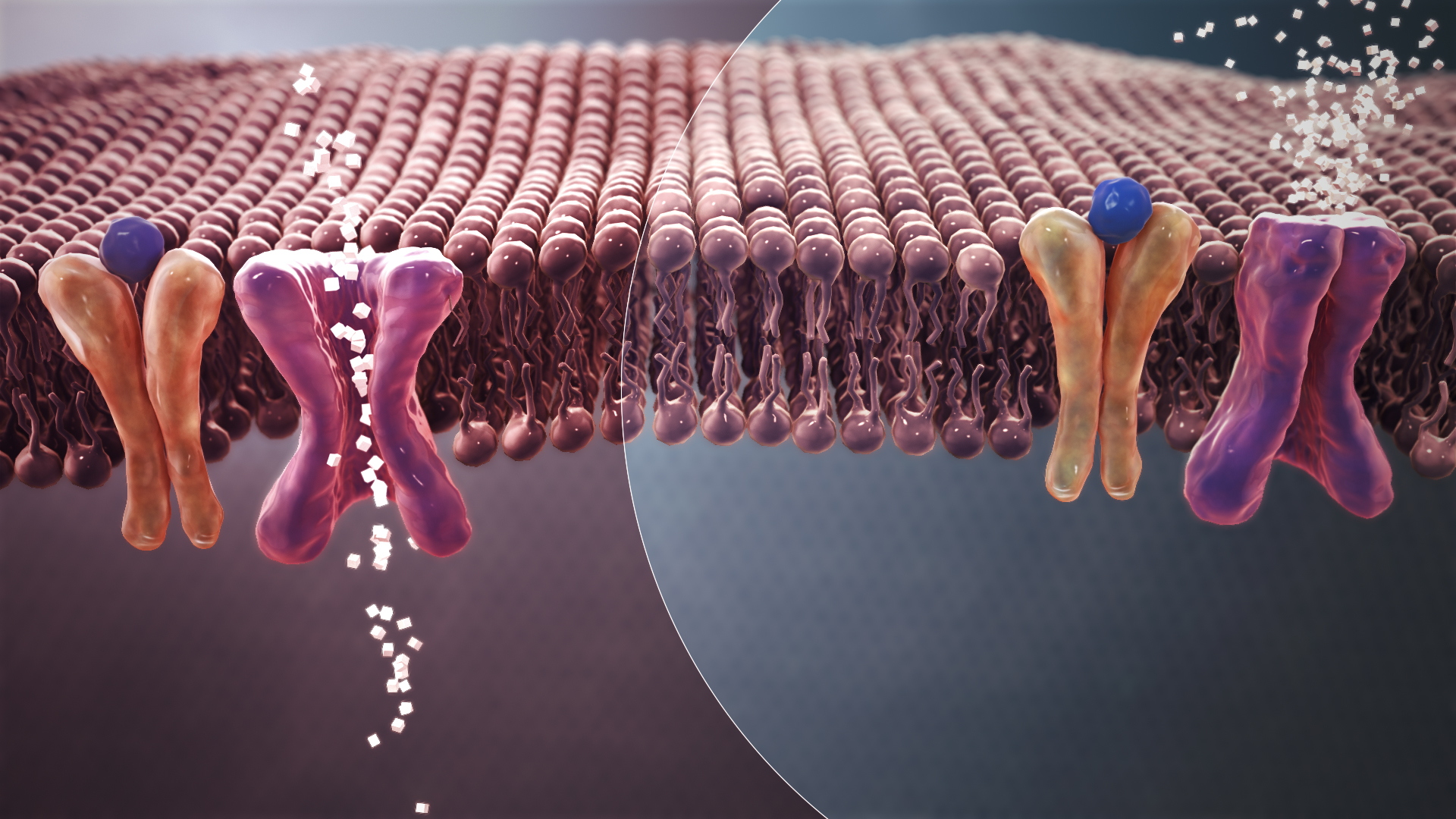
Antipsychotic drugs work by blocking dopamine receptors in the brain. This helps to stabilize mood and reduce psychotic symptoms such as hallucinations and delusions. However, dopamine receptors aren’t limited to the brain; they are also found in other parts of the body including the pancreas, which is the organ of interest in diabetes. When these drugs block dopamine receptors in the pancreas, they can disrupt the delicate balance of hormones that control blood sugar. This can lead to high blood sugar, increased insulin levels, and eventually, type 2 diabetes.
RELATED: Making Antipsychotics with Baker’s Yeast
The New Approach: Protecting the Pancreas
Dr. Alessandro Bonifazi and colleagues published a recent study in the journal Diabetes identifying a potential strategy to reduce the risk of developing diabetes in patients treated with antipsychotic drugs. The researchers proposed that co-administering antipsychotic drugs with drugs that protect dopamine receptors outside of the brain—including those in the pancreas—can help prevent developing type 2 diabetes.
They used a modified version of bromocriptine, a drug already approved by the FDA to treat type 2 diabetes. This modified version, bromocriptine methiodide (BrMeI), is designed to stay mostly outside the brain, activating dopamine receptors in the pancreas without interfering with the beneficial effects of antipsychotics.
RELATED: Learn more about the pancreas in Sweet Solution: Taste Protein Guides Drug Design
What the Study Found
In experiments with mice, the researchers tested BrMeI and bromocriptine. They found that bromocriptine improved blood sugar control when it worked in both the brain and body together. However, when BrMeI’s action was limited to either the brain or the body alone, they did not observe these improvements. This suggests that both brain and body dopamine receptor signaling must be targeted together to effectively manage blood sugar levels.
While this early study on mice showed that BrMeI, when acting only outside the brain, did not have a dramatic effect, it opens the door to designing new drugs that may prevent diabetes without compromising the effectiveness of antipsychotic medications. If this approach is shown to be effective, combining antipsychotic medication with drugs like BrMeI could make it possible to maintain their therapeutic effects on mental health while minimizing their metabolic side effects. It is promising that when bromocriptine acted on both the brain and other parts of the body together, it showed a good effect on blood sugar control. Researchers are still investigating whether this approach affects the efficacy of antipsychotic drugs in the brain.
RELATED: New Chapter in Antipsychotics and Schizophrenia Treatment
Looking Forward
Dr. Zachary Freyberg, a senior author on this research, is currently working with colleagues on the early stages of a safety clinical trial. This trial is to ensure that the therapeutic benefits of antipsychotic medications remain intact when these drugs are administered alongside bromocriptine. The researchers are hopeful that, within the next few years, they will be able to launch a larger trial to test the effectiveness of BrMeI and similar compounds in preventing the impaired blood sugar control often induced by antipsychotic drugs.
Dr. Freyberg highlights the broader implications of their findings: “The fact that both the brain and the body are required to maintain stable glycemic control provides a novel dimension in understanding neuropsychiatry and begins to integrate disparate pieces of knowledge about different organ systems into a coherent whole.”
This study was published in the peer-reviewed journal Diabetes.
The information contained in this article is for educational and informational purposes only and is not intended as health or medical advice. Always consult a physician or other qualified health provider regarding any questions you may have about a medical condition or health objectives.
References
Bonifazi, A., Ellenberger, M., Farino, Z. J., Aslanoglou, D., Rais, R., Pereira, S., Mantilla-Rivas, J. O., Boateng, C. A., Eshleman, A. J., Janowsky, A., Hahn, M. K., Schwartz, G. J., Slusher, B. S., Newman, A. H., & Freyberg, Z. (2024). Development of novel tools for dissection of central versus peripheral dopamine D2-like receptor signaling in dysglycemia. Diabetes, db240175. https://doi.org/10.2337/db24-0175
Featured image: Mechanism of normal Blood Sugar (white crystals) absorption (Left) Vs. insulin resistance in Type 2 Diabetes (Right); by Manu5 and licensed under the Creative Commons Attribution-Share Alike 4.0 International license.

About the Author
Kyle Hewitt is a neuroscientist and third-year PhD candidate at the University of Wollongong, specializing in neuropsychopharmacology. He has a passion for education, which has led to extensive teaching experience in research statistics, biology, biochemistry, pharmacology, chemistry, and scientific literacy. His current research focuses on the interactions between clozapine, extracellular vesicles, and brain immune cells, examining their impact on neuronal function and cognitive processes. His work aims to shed light on how these elements interplay in the context of mental health and therapeutic intervention. Follow Kyle on LinkedIn and X (formerly Twitter).